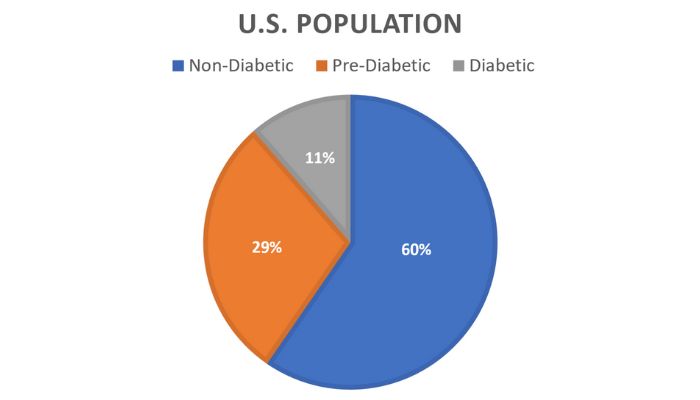
In 2021, the Centers for Disease Control and Prevention (CDC) reported that an estimated 38.4 million adults in the United States are living with diabetes, with 8.7 million of these individuals being unaware of their condition. Furthermore, 97.6 million Americans have been identified as pre-diabetic, including 27.2 million who are 65 years old or older. By 2022, the financial burden of diagnosed diabetes escalated to approximately $413 billion.
Unfortunately, the current healthcare system is more focused on treating illnesses rather than preventing them, requiring individuals to be sick before accessing care. This perspective overlooks the critical importance of preventive healthcare in ensuring long-term wellbeing.

Type 1 diabetes is most commonly diagnosed in children and young adults, occurring when the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. It’s crucial for those with the condition to receive daily insulin therapy to maintain their health. Latest data from the Centers for Disease Control and Prevention (CDC) and the American Diabetes Association (ADA) indicate that approximately 18,200 new cases of type 1 diabetes are diagnosed annually in individuals under 20 years of age. Furthermore, this group has been experiencing an annual increase in cases by about 1.5% since the year 2000. Genetics and environmental factors likely play a role in causing type 1 diabetes.
Type 2 diabetes is the more prevalent form, affecting a significant portion of the U.S. population, often developing in adulthood. This form of diabetes is commonly associated with factors like obesity and a sedentary lifestyle. Recent data from the ADA shows that type 2 diabetes is increasingly affecting younger individuals, with around 5,300 new cases diagnosed each year in those under 20 years of age. In type 2 diabetes, the body either doesn’t produce enough insulin or becomes resistant to insulin’s effects, a condition known as insulin resistance, which can be exacerbated by obesity. Unlike type 1 diabetes, type 2 diabetes can often be managed with lifestyle modifications and medication when necessary.

Gestational diabetes is a form of diabetes that develops during pregnancy, typically in the second or third trimester. This condition arises when pregnancy hormones produced by the placenta affect the body’s ability to use insulin effectively. As a result, the pancreas struggles to meet the increased insulin demands, leading to higher blood sugar levels. Gestational diabetes affects about 1 in 10 pregnancies in the United States. While most women can manage it through diet and exercise, some may require medication. Although gestational diabetes usually resolves after childbirth, it does heighten the risk of developing type 2 diabetes later in life.
Latent Autoimmune Diabetes of Adults (LADA), often considered a variant of type 1 diabetes, typically manifests in adulthood. It involves the immune system erroneously attacking and destroying the insulin-producing beta cells in the pancreas over time. This results in a reduced ability to produce insulin, akin to what occurs in type 1 diabetes. However, LADA’s progression is generally slower compared to the type 1 diabetes that develops during childhood. While LADA is not classified as a distinct type of diabetes, it shares characteristics with both type 1 and type 2 diabetes. Often, LADA is initially misdiagnosed as type 2 diabetes in adults, accounting for a significant number of these cases. Most people with LADA will eventually require lifelong insulin therapy, although some may initially manage their diabetes with oral medications beforehand.
Type 3 diabetes is used informally and primarily for research purposes to explore the potential links between diabetes, particularly type 2 and Alzheimer’s disease. It’s a term sometimes used in research to describe cases where diabetes and dementia or Alzheimer’s disease occur together. Some studies have found a potential link between long-term high blood sugar, from diabetes, and an increased risk of cognitive decline. Type 2 diabetes doubles the risk for developing Alzheimer’s disease. This is likely due to the fact that in both diabetes and Alzheimer’s disease, there is a deficiency of insulin signaling. However, more evidence is still needed before diabetes related to dementia would be classified as a distinct third type.
Treatment focuses on managing blood sugar through diet, exercise, medication including insulin therapy, and monitoring blood sugar levels. Diabetes management is important to prevent health issues and live a full life.

Request a consultation
Add what your body needs
Vitamins & Minerals
Take advantage of mother nature
Fresh food for your body